“I am terrified to visit the public clinic. What would happen if people found out I’m having sex, or if they thought I’m HIV positive?” This is a quote from “Mamello,” a young woman in Maseru, Lesotho. Mamello lives with her parents. She has a boyfriend who is her age, but she also has an older sexual partner who often gives her money. While there is a nurse at her school, Mamello is unable to access personalized sexual and reproductive health services on school premises due to local guidelines. Instead, she has to wait until after school to go to a clinic, but rarely has time and is nervous to go at all, for fear of societal and family repercussions.
This situation is common for adolescent girls and young women (AGYW) in Lesotho, where family involvement, social stigma and pressure, and lack of convenient access hinder initiation onto and continuation of oral PrEP for HIV prevention. In fact, there is a growing trend amongst broader populations in lower middle income countries (LMICs), not just AGYW, for a desire for enhanced privacy, convenience, confidentiality, quality, and consistent supply in health products and services that has led many to seek care in non-traditional spaces, such as private pharmacies, clinics, or drug outposts. The Center for Innovation and Impact (CII) within USAID’s Bureau for Global Health, in partnership with the Office of HIV/AIDS and USAID/Lesotho saw an opportunity to further the use of the private sector to create new, decentralized access points to decrease barriers to HIV prevention services. CII’s expertise in innovation, private sector engagement, digital health, and human-centered design (HCD) led to a desire to explore and enhance private sector linkages to increase access to oral PrEP. Building on the appeal of V, an oral PrEP brand and service model delivery strategy originally co-created with AGYW and healthcare workers in South Africa and currently being piloted in Zimbabwe, CII identified the vast potential of HCD to improve the user experience, design more appropriate products and service model delivery strategies, and elevate the voice of the user in her own health journey.
Setting up an innovative and diverse project team
Given the generalized HIV epidemic and high HIV incidence rates in Lesotho, the country was a natural choice for this type of work. As Lesotho approaches epidemic control (at 90-97-92 progress towards UNAIDS targets to end the AIDS epidemic), PrEP is a key intervention for HIV prevention and a priority strategy for PEPFAR. PEPFAR/Lesotho is committed to sustaining the gains that have been made, making the country particularly well suited for an innovative project focused on HCD and private sector engagement for PrEP among AGYW.
CII convened experts in HCD, private sector engagement, and PrEP to accelerate impact in Lesotho, leveraging existing structures and local partners in order to ensure this work was sustainable and could be readily implemented. After identifying that the Office of HIV/AIDS at USAID and the USAID Mission in Lesotho were interested in increasing AGYW PrEP uptake and exploring non-traditional access points to increase access, de-medicalize and destigmatize PrEP, CII embedded an HCD team in an existing USAID mechanism, EpiC, that was already exploring private sector access points for HIV products. Leveraging the expertise of partners in the EngageDesign consortium and partners working in Lesotho such as Jhpiego, Right to Care, FHI360, EGPAF, Karabo, and Baylor, we set out to map the journey of PrEP awareness, access, and continuation for different sub-groups of AGYW in Lesotho.
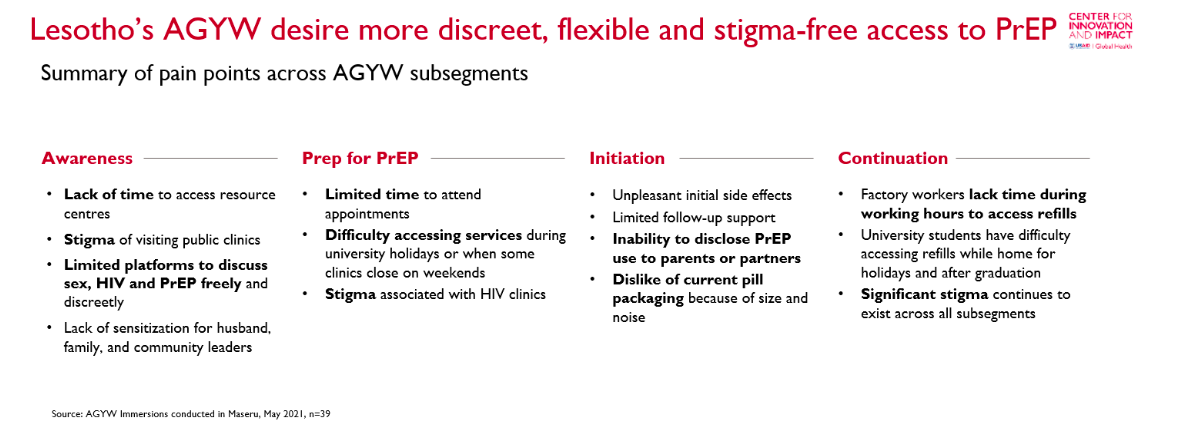
Barriers to accessing PrEP among AGYW
Building on the existing evidence base and through in-depth HCD interviews with AGYW in Lesotho, it became clear that AGYW face a litany of obstacles in accessing PrEP along their “journey” as a consumer (summarized in Figure 1. below). Common across the entire journey are potential stigma and limited time. As young, healthy women, AGYW are hesitant to seek out health information, visit clinics, and take medication related to HIV. In particular, AGYW living with their parents, or those who are married, worry that someone may see them queuing at the HIV clinic and their parents, husbands, or in-laws would find out. Younger AGYW worry that their parents would not approve of them having sex, while married AGYW do not want their husbands to assume they do not trust them or are having sex with another partner. They feel the conspicuous pill bottles and rattling would make it especially difficult to hide. AGYW that work in factories are constrained by limited breaks and strict schedules that make it difficult to initiate on PrEP or pick up oral PrEP refills during the day. All population segments of AGYW cite lack of time as a barrier to accessing PrEP, particularly because many health facilities are often closed in the evenings and on weekends.
Figure 1. Summary of AGYW pain points in accessing PrEP
A new way to access PrEP via the private sector
To address these identified pain points, we imagined what a better PrEP journey might look like for AGYW, and tested these ideas directly with AGYW. The key features of this new PrEP journey seek to address the main pain points identified in conversations with AGYW.
- It helps reduce stigma and improve privacy by bundling PrEP with other products.
- It also improves convenience, by offering initiation and continuation services in the convenient private sector locations AGYW already frequent, as opposed to HIV-specific sites.
- Relatable PrEP buddies provide them support across the entire journey to address concerns that may arise related to side effects or access.
The near-term program (Figure 2. below) will be implemented as a “minimum viable” solution that addresses key pain points in a low-complexity way.
Figure 2. Key components of new private sector PrEP journey
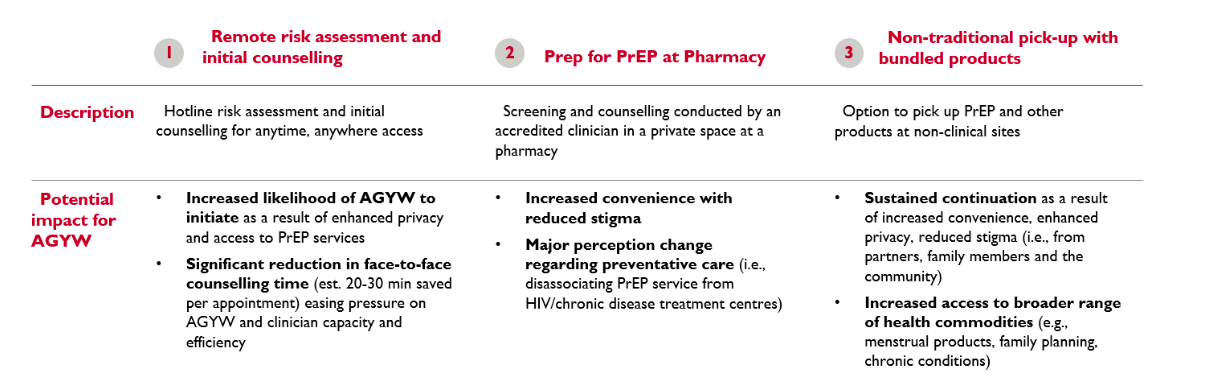
The solution consists of 3 main components:
-
- Remote risk assessment and initial counseling: AGYW can call a convenient, toll-free hotline which links them directly to accredited staff such as nurses/clinicians. They can learn about this hotline via sources such as information cards with the toll-free phone number, website address and printed QR codes distributed at youth centers and in the community by personnel such as Jhpiego’s Voluntary Counselling Advocates (VCAs) or peer educators. If they complete the screening process and are found to have high-risk behaviors for HIV infection, they will be given clear next steps and directed to their preferred pharmacy for counseling and initiation. To support navigating these initial steps, they will be connected to a trained and compensated peer AGYW – “PrEP Buddy” – to ensure they can successfully access the pharmacy and address other questions or concerns they may have.
- Prep for PrEP at a pharmacy: When they access the pharmacy, they will have an appointment in a private space with a trained, accredited nurse/clinician to receive initiation counseling and PrEP prescription. The pharmacy systems will feed data into the MoH reporting systems as required to ensure proper tracking and linkage into public sector data systems.
- Non-traditional pick-up with bundled products: Once they have received their initial prescription, AGYW can access subsequent refills via non-traditional, private sector channels, including pharmacies. Depending on the resource requirements, they may also be able to access PrEP at automated lockers (such as the Collect & Go lockers created by Right to Care) located at universities, malls and youth centers, or through alternate delivery services. They will have the option to pick up PrEP on its own, or bundled in a package with other health-related commodities such as menstrual products or, as available, family planning commodities.
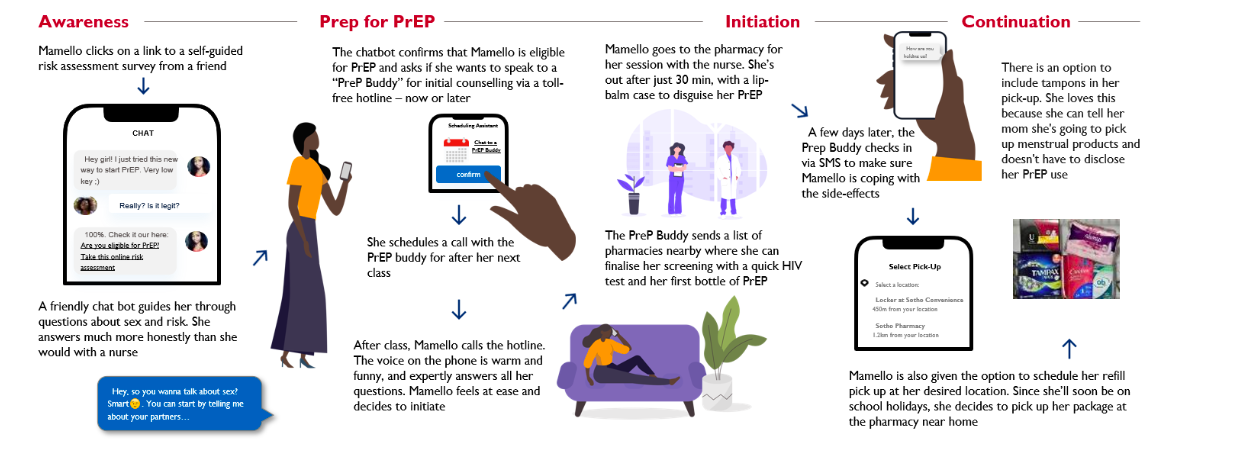
In the longer-term, an aspirational journey might look like Figure 3. below. This solution builds on the key features outlined above with several more complex features that will require more time and resources to build prior to roll out. In this aspirational journey, a young woman is able to take a chat-bot guided risk assessment, and if she is found to have risk behaviors for HIV infection, she is directly connected with a trained AGYW “PrEP Buddy” for more customized questions and support. For refills, she can pick up her prescriptions via automated lockers in convenient locations such as malls, along with other health product needs such as family planning or menstrual hygiene products.
Figure 3. Aspirational AGYW PrEP journey
Making the new journey a reality
As we designed this new PrEP offering, we worked closely with existing PEPFAR implementing partners in Lesotho through a series of interviews and workshops. These conversations enabled us to identify how to integrate different aspects of the solution into existing programs and validate capacity requirements and gaps. This close coordination was critical to ensure feasibility of the new solution and increase the likelihood of implementation.
The new journey will be rolled out over the coming year, with the support of several partners already implementing PrEP for AGYW in Lesotho. The EpiC consortium (FHI360, Right to Care, Gobee Group, Population Services International, and Palladium) will oversee the end-to-end solution, as well as the supply chain and infrastructure requirements for pharmacies. Jhpiego will design and implement the screening hotline service and will identify, train, and support pharmacy-based nurses to prescribe and counsel AGYW on PrEP. For each of the use cases, the team is looking at the economics holistically, compiling the major cost drivers (e.g., digital tool/platform development, personnel remuneration, etc.), funding and resourcing considerations (e.g., donor/MoH funding for digital platform, access to commodities supply chain, etc.) and monetization potential (e.g., offer risk assessment tools as media buying platforms, differentiate “premium” services for a fee) in an effort to drive improved uptake and adherence, and ensure sustainability over time.
Scaling across countries, populations, and products
The key findings and recommendations from this project are applicable far beyond oral PrEP (i.e. to other PrEP products like the dapivirine ring, potentially CAB LA, and even beyond PrEP), the country of Lesotho, or AGYW population. In many LMICs, users are seeking ease of access to health services in more convenient locations, with greater levels of confidentiality, and through digital services that fit their lifestyles. In many instances, the private sector is perfectly suited to achieving these goals. Non-traditional pickup or refill points for health products such as malls, transit stations, schools, workplaces, or community centers can help populations feel less stigma in seeking care or give them the time or ease of access they never had before. Given the context of COVID-19, these pickup points also create safer, more convenient options to access products outside of a health center. Bundling these products with other medicines such as diabetes or pain medication and other supplies such as menstrual hygiene or family planning products can make it even easier for patients.
Learnings from this project can be used to more effectively de-medicalize and destigmatize products across the entire HIV continuum of care, as well as other diseases. Focusing on the entire user journey, from end-to-end, can help countries, partners, and donors design more appropriate, relevant, and accessible products and processes that enhance uptake and adoption, leading to better health outcomes. Whenever possible, future projects and programs should seek to incorporate HCD lessons and insights from previous work to improve scale (such as how this project leveraged the “V” findings to make recommendations for AGYW in Lesotho), but also ensure that local needs and specific populations are tailored to. When designing products and services for younger populations, it is critical to design with these users and capture not only what they need, but what they want.
The views expressed in this article do not necessarily represent the views of USAID or the United States Government.